Robots don’t have feelings. The Cartesian, assembly, and palletizing bots that have replaced the human workers of yesteryear don’t need to sense a thing to do their jobs.
Not so the surgical robot. Machines that arrange flesh need be more delicate beasts. Surgeons that control robots within a human body have had to guide their machines without the tactile sense, at a time and place where such a sense would seem crucial. “You have these hemostat-looking devices that go and grip tissues,” says Jason Clark, the vice president of engineering at Cambridge Research and Development. “It’s a very delicate process. You’re driving a robot that has way more power than is really necessary. So when you’re grabbing a piece of tissue you can damage it or restrict blood flow and ruin the tissue really quickly.”
Pneumatic Solution
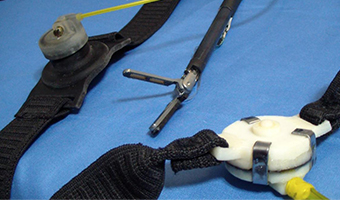
Clark and his colleagues knew there had to be a way to give a surgeon the feeling from the tip of a robotic tool. His solution is a small circular diaphragm that can be strapped on anywhere on the body. A pneumatic protuberance extends like a finger to prod the surgeon as the tool he’s using prods, or grips, flesh.
To do so with enough smoothness and what could be called “pressure resolution,” Clark and his colleagues went through many iterations. “It can’t be digital or herky-jerky,” says Clark. “It has to operate smoothly, a person has to easily perceive change.” Clark tried muscle wire, but it lacked the necessary resolution and power. Early pneumatic solutions didn’t react fast enough. “We tried something that was mechanical, a servo motor that was cable-driven, like bike brakes. Pull on a cable and it would move a plunger that would apply pressure to your skin,” says Clark. “That was OK, but you would feel the motor transmitting up the wire. It wasn’t perfect.”
Eventually the team settled on a two-part pneumatic solution. On one side of the actuator is a sealed column of air. On the other side, a fill solenoid and an empty solenoid work with open air. The result is a smoothly changing 254 degrees of pressure. When worn, the surgeon, or anyone who might try, quickly learns to interpret the prodding of the device as feeling from the end of the surgical tool. “While forcing a needle through tissue, they are holding it with a gripper. There’s now affirmation that they are gripping the needle,” says Clark. “They have the ability to say, ‘Yeah I have that needle.’”
Sense of Touch
With that problem solved, Clark turned his attention to getting some sensors on the ends of a few surgical tools. That, however, turned out to be not so simply done. “Here we are building this haptic feedback device, focusing on the part that touches you, and we come to find out that the larger challenge was the sensors. We thought to ourselves, at the beginning ‘There’s a million sensor solutions out there, we’ll just go out and get a sensor,’” says Clark. It turned out that there were no off-the-shelf sensors small enough, and there were no appropriately accommodating surgical tools either. “We had to go and design some tools that have resistive and capacitive sensors.”
Those tools, destined to do their work in a human body, have to be packaged and sterile or capable of being autoclaved and surviving 300 degree heat. “We’re marching down the road of a disposable sensor,” says Clark. It has to be cost-effective, you have to be able to throw it away and not have it cost $300.” Regardless of the current cost, this April, surgeons at Boston Children’s Hospital that Clark has been working with performed the first simulated blindfolded procedure.
Clark hopes to eventually have sensors that do and feel more than what a surgeon's fingers might be capable. If a sensor could detect the density of a material, surgeons might be able to “feel” the difference between good and bad tissue. “They could literally take the scalpel and make cuts to remove that bad tissue. It’s nothing more than a tool with a tip with sensors,” says Clark. “But how is cool is that? To affect the outcome of a surgery like that.”
The haptic device may have applications beyond the surgical, and can be used anywhere a robot would better do his job with a sense of touch. Underwater robots could better fix leaking oil pipes, say, bomb-sniffing robots could let their operators better feel the tension of wires they were disassembling, UAV pilots could feel pitch, roll, and yaw.
“More and more robots and technology are replacing the human element. What you’re taking away is that sense of touch,” says Clark. He and his colleagues are putting touch back where it belongs.
Source: asme.org
Look at the technology now, you don't know what new at what will be invented that very useful to us.


No comments:
Post a Comment